Sonali Bajaj1, Neha Sharma1, Abhinav Anand1, 2, Devesh Tewari1, Navneet Khurana1, *
1 School of Pharmaceutical Sciences, Lovely Professional University, Phagwara, Punjab, PIN- 144 411, India
2 CT Institute of Pharmaceutical Sciences, CT Group of Institutions, Shahpur, Jalandhar, Punjab, PIN- 144 020, India
Abstract
The recent emergence of the novel betacoronavirus, pathogenic severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) with high nucleotide identity to SARS-CoV represents the causative agent of a potentially deadly disease coronavirus disease-19 (COVID-19) in Wuhan, China, and spreading across several countries globally pose a great global public health concern. Until a vaccine is available, effective therapy must be identified, and many clinical trialshave been executed worldwide. Various in vitro investigations are ongoing using different cell cultures to find alternative treatment options, allowing SARS-CoV-2 replications. Various cell lines are susceptible to the SARS-CoV-2 infection. In this chapter, literature regarding SARS-CoV-2 isolated in several cell lines commonly used for diagnostic or research purposes has been summarized. It also shows that SARS-CoV-2 can achieve high titers in various cell cultures derived from different species. In addition, these cell lines are extensively used in the diagnosis, to study pathophysiology, genome studies, and the finding of new targets for drug development and provide new ideas for the discovery of lead compounds with potential therapeutic agents against novel COVID-19.
Keywords: Anti-viral, Betacoronavirus, Cell lines, Clinical trials, Lead compounds, SARS-CoV-2.
* Corresponding author Navneet Khurana: School of Pharmaceutical Sciences, Lovely Professional University, Phagwara, Punjab, PIN- 144 411, India; E-mail: navi.pharmacist@gmail.com
INTRODUCTION
The first outbreak of the novel coronavirus occurred in Wuhan on December 12, 2019, in China, and abruptly spread to several other nations. The World Health Organization (WHO) declared a name for 2019-nCoV infectious disease coronavirus disease-19 (COVID-19) on February 11, 2020. The virus name was renamed Severe Acute Respiratory Syndrome-coronavirus-2 (SARS-CoV-2) by the International Committee of Taxonomy of Viruses, earlier called 2019-nCoV [1].
During the last 20 years, three infectious diseases, such as SARS and the Middle East Respiratory Syndrome (MERS), have been triggered by coronaviruses.
This suggests that COVID-19 is not the first infection caused by coronavirus [2]. According to the classification of the CoVs, it belongs to the Coronaviridae family having Coronavirinae subfamily of the Nidovirales order, which their subfamily comprises of 4 genera coronavirus, namely α, β, γ and δ [3]. The nucleotide arrangements of the SARS-CoV-2 were associated with SARS-CoV and MERS-CoV that demonstrated greater homology to SARS-CoV, although they were comparably weak with the MERS-CoV [4]. It is not surprising that many researchers have newly verified the genomic similarities associated with the SARS-CoV-2 and bat betacoronavirus, which belongs to the sub-genus Sarbecovirus [5]. The researchers have also found that the SARS-CoV-2 utilizes the identical receptor known as the Angiotensin-Converting Enzyme 2 (ACE2), similarly to the SARS-CoV [6]. Tyrell and Bynoe first identified the coronaviruses in 1966 and grown the viruses by taking samples of the patients suffering from the common cold [7]. The enclosed, positive single-stranded giant RNA viruses of about 30 kb in size are the characteristics of coronaviruses that infect individuals and the wide-ranging of creatures. Genomic sequencing of the SARS-CoV-2 has already been done. It has been found that the SARS-CoV-2 has originated from the bat that emerged from a photogenetic study [8]. Entry of this virus into the host organism is facilitated with the transmembrane S-glycoprotein (spike), which makes homotrimers protruding from the virus's surface.
Currently, no approved treatment is available for managing COVID-19. There are no specific drugs for the treatment, so there are many supporting measures that are usually given to the patients, including oxygen treatment, antimicrobial agents, antifungal drugs, and Extracorporeal Membrane Oxygenation (ECMO), etc., [9]. This chapter aims to comprehensively gather all the medical literature highlighting the various cell lines that are useful in replicating SARS-CoV-2 that can be fruitful for in vitro studies of an anti-viral drug effective in managing COVID-19 disease. Also, not only for evaluating the anti-viral drugs but also for these cell lines are useful for various purposes. For instance, to study the pathogenesis, study the genome of this virus, and find the new targets for drug development is important to highlight.
Role of Cell Lines in Scientific Research
Instead of individual cells, immortal cell lines are also used to explore the plethora of biological processes. The benefits include cost-effectiveness, easy-to-use, limitless availability of products, and it avoids the ethical questioning involved with human and animal tissues [10]. In vaccine development, monitoring of the drug metabolism and cytotoxicity, antibody development, the analysis of genetic material regulation, and artificial tissue creation, in addition to the development of biological substances such as therapeutic proteins and cell lines, have revolutionized medical science [11]. Traditionally, the diagnosis of the viral disease has focused on viral pathogens in cell culture isolation. Even though this technique is always sluggish and needs significant scientific skill. The laboratory diagnosis for the viral disease has been recognized as a “gold standard” for decades. Cell lines are extracted from cells separated from the original tissues after broken down through various methods, including enzymatic, mechanical, or chemical. It has been given a huge quantity of cells appropriate for isolation, allowed the monitoring that helps reduction in the use of laboratory animals, and has contributed to antibiotic and clean air pollution [12]. However, in confirming the causative agent of the disease during high prevalence, the culture of cells has always been essential [13]. In current years, however, technical advances, from monoclonal antibody production to molecular diagnosis, have created powerful methods useful in detecting the various forms of viruses. Molecular identification of viral deoxyribonucleic acid (DNA) and ribonucleic acid (RNAs), molecular multiplication using Polymerase Chain Reaction (PCR), and additional methods in diagnostic laboratories have become increasingly usable. Using an RT-PCR multiplex for SARS-CoV detection, scientists evaluated several human and animal cell lines [14]. The goals of the RT-PCR (real time-PCR) technique are:
1. Glyceraldehyde 3-phosphate dehydrogenase, as an internal RNA integrity regulation and help in the development of cDNA.
2. For the input virus identification process, SARS-CoV genomic RNA is targeted.
3. It also showed the 3' co-terminal specific sub genomic RNAs representative of viral ingestion and appropriate for the viral replication initiation process.
As the SARS-CoV is extremely pathogenic, most laboratories are unwilling to separate this virus in culture. Because of the high pathogenic nature of these viruses, co-cultured cell lines serve as the best alternatives, for instance, R-Mix (Diagnostic Hybrids, Inc.). R-Mix is a blend of the mink pulmonary cells and human adenocarcinoma cells, consisting of the strains Mv1Lu and A549, respectively [15].
Table 1 Summary of the different cell cultures with their species of origin and cell type.
|
Cell Line |
Species of Origin |
Cell Type |
|
Caco–2 |
Homo sapiens |
Colon carcinoma |
|
Huh-7 |
Homo sapiens |
Liver hepatocellular carcinoma |
|
A549 |
Homo sapiens |
Lung carcinoma epithelium |
|
Intestinal organoids |
Homo sapiens |
Intestinal epithelium |
|
HAE |
Homo sapiens |
Airway epithelium |
|
HEK-293 |
Homo sapiens |
Fetal kidney |
|
Calu-3 |
Homo sapiens |
Bronchial epithelium |
|
Vero |
Chlorocebus aethiops |
Kidney epithelium |
|
Vero E6 |
Chlorocebus aethiops |
Kidney epithelium |
There are nine different types of cell lines used in the culturing of SARS-CoV-2, which include Caco–2, Huh-7, A549, intestinal organoids, HAE, HEK-293, Calu-3, Vero, and Vero E6 as shown in Fig. (1) and Table 1. All cell lines originate from the human cell cultures except Vero cell lines obtained from kidney epithelium cells of African green monkeys. Human cell cultures include; colon carcinoma, hepatocellular carcinoma, lung carcinoma epithelium, intestinal epithelium, airway epithelium, fetal kidney cultures, and bronchial epithelium.
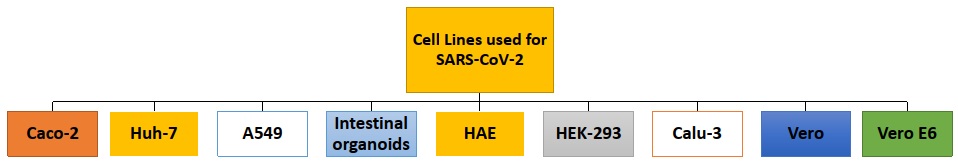
Fig. (1))
Various cell lines used for the SARS-CoV-2 replication.
Caco-2 cells
In 1977, Fogh and his colleagues developed the cell culture Caco-2 from a human colon adenocarcinoma to assess anticancer medications' cytotoxic effects and evaluate the various pathways of drug resistance [16]. Across several scientific fields like pharmaceutical science, intestinal epithelial cell lines, including Caco-2, have increased significantly in recent years. The initial experiments on the Caco-2 lines indicate that the cells display a wide range of morphological and biochemical features of small intestine enterocytes after differentiation. This model has become a standard way of predicting human absorption of intestinal drugs and mechanisms underlying the drug transport experiments [17]. The cell's surface confronting the top medium forms a brush border similar to the intestinal epithelium's luminal membrane. The cell surface that binds to the permeable membrane and faces the lowermost medium is transformed into the basolateral membrane [18]. These Caco-2 cell cultures are usually grown in monolayers, display a cylindrical polarized structure, microvilli on the apical surface, tight junctions among neighboring cells, and exhibit hydrolase enzyme activities on the surface of the apical membrane. However, these activities of the hydrolase enzymes in the human fetal colon are identified to be transiently expressed in the 15th week of their pregnancy. It was observed that in the adult human colon, such hydrolase enzymes are absent. Further research on the features of the Caca-2 differentiated cells in the enzyme indicated that they are more similar to the fetal than to adult ilea intestinal absorptive cells [19]. Numerous transporters as well as receptors and enzymes that are involved in the metabolism namely, sulfotransferases (SULTs), UDP glucuronosyltransferases (UGTs) and glutatathione- S- transfers (GSTs), and cytochrome P450 1A (CYP1A) are involved in the Caco-2 cell lines [20].
These cell lines support various types of viral replications. Recently, Caco-2 cell cultures are utilized in the culturing of the SARS-CoV-2 collected from human samples. The efficacy of the Darunavir, which is an oral nonpeptidic HIV-1 protease inhibitor for the treatment of COVID-19, was assessed. But, it was found by the researchers that Darunavir fails to show anti-viral activity in the SARS-CoV-2 infection [21].
Huh-7 cells
The related cell cultures used in in vitro research are varied in their genetic and phenotypic profiles, as are human hepatocellular carcinoma (HCC) [22]. For instance, differential proliferative response to Src /Abl blocker in HCC cell cultures, i.e., dasatinib [23], and growth factor-β such as transforming growth factor-beta (TGF-β) stimulation are known [24]. A permanent cancer cell line from the hepatoma tissue, which was operatively removed from a Japanese patient of 57 age in 1985, is Hereafter Huh7 (HuH-7) [25]. It is worth mentioning that Huh-7 cell lines were the long-sought-out cellular system that is permitted full molecular research related to the Hepatitis C Virus (HCV). In several investigations, including research related to iron metabolism, Huh-7 cells have been extensively used and support various viral replications [26].
As a conventional Chinese drug, Lianhuaqingwen (LH) has been used to manage influenza and had a wide-spectrum anti-viral activity on several influenza viruses. It is also used in the regulation of the immune system of the body [27]. The recent in vitro investigation of LH has been done to find effectiveness in treating the novel SARS-CoV-2 virus and possible effects on the regulation of the human immune system. In the cell culture of Huh-7, pro-inflammatory cytokine expression levels were assessed by real-time quantitative PCR screening against SARS-CoV-2 infection. In contrast, its anti-viral effects were determined by the Vero E6 cells. These findings suggest that LH shows an anti-inflammatory effect due to decreases the release of the cytokine from the host cells and halts the virus replication [28]. Besides, Huh-7 cells are used in the culturing of SARS-CoV-2 in the plethora. For instance, Huh-7 is used to evaluate the susceptibility of T- lymphocytes in SARS-CoV-2 infection [29] and the examination of the viral architecture of SARS-CoV-2 with the help of electron microscopy [30].
A549 cells
Different forms of cells, including alveolar type I and type II, lead to the pulmonary barrier. Type I cells occupy about 96% of the pulmonary epithelium surface and therefore cannot be segregated. Type II cells have several different roles, even as they occupy a much smaller surface region of the alveolus [31]. In parts of the lung tissue, alveolar cells of type II may be recognized by their characteristic morphological features, the typical pattern of staining using histochemical dyes, and a distinct cytoplasmic organelle. It has multilamellar bodies, a single membrane, and electron-rich materials are the two characteristics features of the suicidal bags, i.e., lysosomes [32]. These type II cells are susceptible to the numerous microbes. These can enter the air sacs of the lungs and be infected by multiple viruses and bacteria, namely influenza virus, SARS coronavirus, Legionella pneumophelia, Bacillus anthracis, or Mycobacterium tuberculosis, which has a capability of replication and survival within type II alveolar epithelial cells [33].
Moreover, most human tumor cell line A549 were done, which is known as the human model of type II alveolar epithelial cells. The cell cultures A549, which was developed in 1972, were taken from the cancerous human alveolar cell and had pulmonary epithelial Type II cells, like lamellar bodies [34]. The ultrastructure of A549 cells has reported various morphological features including, the diameter of the cells were 4.93 µm and 10.59 µm. It was estimated with the help of inverted microscopy and transmission electron microscopy, respectively, and the total volume and surface area of suicidal bags, i.e., lysosomes, were 21.69 µm3 and 212.04 µm2, respectively [35]. The A549 cell line is an excellent model in many aspects since the endocytic role and localization of cytochrome P450 systems primarily depend on the alveoli's surface epithelial type II cells. A549 cell cultures do not exhibit any functional tight junctions between neighboring cells [32].
Comparative study of host transcriptional response by the SARS-CoV-2 with the seasonal Influenza A Virus (IAV) along with human orthopneumovirus (usually called human Respiratory Syncytial Virus (RSV), which is achieved by infecting A549 cells with these three viruses. Data showed a unique transcriptional response, as it does not contain Type I and III interferons (IFN). Also, secreted peptides involved in respiratory disease are the only genes that seem to be distinctive to the SARS-CoV-2 infection [36].
Atazanavir is the first once-daily protease inhibitor (PI) that is licensed in several nations marketed as a therapeutic agent in the Antiretroviral Therapy (ART) regimens in the management of adults, and in certain nations in pediatric, also for patients who are suffering from the HIV-1 infection [37]. SARS-CoV-2 infection was managed via atazanavir as a therapeutic agent. In vitro research was performed in which A549 cell lines are infected with the SARS-CoV-2 virus. Findings revealed that reduced interleukin-6 (IL-6) levels in SARS-CoV-2 human primary monocyte and cellular mortality and cytokine storm-linked mediators decreased. Mortality of the patients with SARS-CoV-2 infection linked with the increased levels of IL-6 and apoptosis. Research points atazanavir as a new alternative among commercially approved medicines to be considered for successfully managing SARS-CoV-2 infection in ongoing clinical trials [38].
Human Intestinal Organoids
In adult mammals, epithelial cells of the intestine are the quickest in dividing and regenerating various tissues. Intestinal epithelium regeneration is strictly regulated with the help of intestinal stem cells (ISC) and self-renewal [39]. Histologically, epithelial cells of the small intestine are partitioned into two sections:
1. The crypts
2. The villi
Crypts are predominantly made of the proliferative compartment and contain undifferentiated cells, including transit amplification cells and ISCs. Within this area, the epithelium ensures a significant cell turnover and protects the stem cell's niche [40]. On the other hand, villi are a functioning compartment in the epithelial cells that include differentiated cells that lose the power of multiplication and have the characteristics of the developing epithelium. These segregated epithelial cells comprise the villi and can be classified depending on their role such as enterocytes that act to absorb nutrients, goblet cells involved in a defensive mucus layer, and cells of enteroendocrine that produce gastrointestinal hormones [41]. The ISCs regularly regenerate themselves throughout the individual's life cycle and contribute to all sorts of distinct tissue lines. Experiments including genetic lineage tracing systems have presented that the columnar cells present in the crypt region, recognized by the expression of Leucine-rich repeat-containing the G protein-coupled receptor 5 (Lgr5), act as ISCs [42].
Researchers have developed stem cells in vitro for many years, driven both by fundamental scientific research and therapeutic goals. Ten years ago, Sasai showed that apart from leading the pluripotent stem cells into a certain lineage, they obtain distinct cell populations. Their stem cells and progeny may follow and organize themselves into similar structures representing several histological and functional aspects of actual organs [43]. The advancement of organoid technology has been scientifically transforming with vast applications in the different research areas, including epithelial and cell biology and clinical applications like organoid biobanks derived from the patients [44]. Such in vitro organ mimetic is labeled as organoids. The source of the extracted tissue often determines the structure and characteristics features of the subsequent organoid when it refers to intestinal organoids [45]. Organoids are extensively used in studying various host-bacterial pathologies and used in studies associated with the commonly occurring and problematic pathogens so that new drug targets can be found. In the U.S, for the management of diarrhea which is caused by Clostridium difficile, at an annual expense to healthcare approaching 1 billion US$ per year was estimated [46]. The illness caused by Clostridium difficile and also to study the various pathologies associated with it, numerous immortalized cell lines are widely used. However, organoid production has made it possible to validate existing theories and further helps in the improvement in the cellular mechanisms related to cytotoxicity [47].
While the clinical manifestation of COVID-19 comprises majorly respiratory symptoms, a minority of patients report gastrointestinal symptoms [48]. In addition, the diagnosis of the COVID-19 rectal swab can be used as it showed the presence of viral RNA [49], even after the nasopharyngeal screening is showing negative results. So, it suggests a pathway of transmission of gastrointestinal and fecal-oral infection [48].
The first in vitro culturing of Norovirus was done with the help of the Human Small Intestinal Organoids (hSIOs) [50]. To discover the pathway of SARS-CoV-2 that is followed during the transmission of gastrointestinal and fecal-oral infection, researchers cultured ileal hSIOs in four distinct culture mediums. These include 'High Expansion Medium (EXP)', 'Differentiation Medium (DIF)', 'Differentiation Medium-Basic Metabolic Panel (DIF-BMP)' and 'Enteroendocrine Cells (EEC)' which help in the amplification of the virus. hSIOs cultured with a significant proportion of stem cells and enterocyte progenitors in the WNT- EXP. DIF is used to culture organoids, including enterocytes, goblet cells, and a very small number of EECs. BMP2/4 incorporation to the DIF (DIF-BMP) further helps in differentiation and the growth of the cells [51]. It was reported that the SARS-CoV-2 virus utilized the identical receptor, which SARS-CoV already uses, i.e., ACE2, and this receptor is found in the differentiated enterocytes. The study found that enterocytes were readily infected by these two viruses, i.e., SARS-CoV and SARS-CoV-2 which was displayed by the help of the confocal and electron-microscopy in the hSIOs. As a result, significant titers have been identified as infectious viral particles. The mRNA expression screening indicates that the available viral response system has been highly induced. It is stated that hSIOs serve as in vitro models for coronavirus infection. These organoids support multiplications of the SARS-CoV-2 and may be utilized in the findings of the pathogenesis of the COVID-19 disease [52].
HAE cells
The nasal cavity, trachea, and bronchi are lined by the epithelium, which acts as a prominent part in defending the host from several harmful substances such as chemical and particulate contaminants and infections [53]. Foreign particles are stuck in mucus on the surface of the mucus membrane and expelled via coordinated beating of cilia and/or coughing. Airway inherent host protection involves physical trapping and elimination of toxic compounds associated with baseline or inducible release of antimicrobial agents, antioxidants, and protease blockers and the mobilization of non-specific immune cells that includes neutrophils and monocytes [54]. Epithelial cells of the air sacs have thin and wider surface area which is guarded via alveolar macrophages, and this epithelium composed of has a pseudo-stratified surface consisting of a total of six different forms of epithelial cells [55]: a) Ciliated, b) Mucous, c) Clara, d) Serous, e) Basal and f) Dense core- granulated.
Cancer and cystic fibrosis (CF) study are the two key factors behind the production of human airway epithelial cell cultures (HAE) [56], which is stimulated by the shortage of tissue. Scientists have now established a range of specified systems for cell culture, which involves the biochemical and genetic factorsaffecting these and many other airway diseases [57]. Retroviral and lentiviral vectors are the main components of the HAE study toolbox, and many researchers can access their development through individual laboratories. Through collaborating surgeons and pathologists with the appropriate institutional, local and national guidelines, airway epithelial cells may be removed from trachea or bronchi, nasal turbinate, or polyp specimens [54].
In HAE models, airway architectural design and cellular complexity are easy to infect with various human and Zoonotic CoV, such as SARS-CoV and MERS-CoV [58]. In recent investigations, HAE models were used to assess the potential of the various anti-viral drugs in managing the SARS-CoV virus. One of the broad actions as an anti-viral agent ribonucleoside analog β-D-N4-deoxycytidine (NHC, and EIDD-1931) is used to treat the distinct RNA viruses, namely influenza, Ebola virus, CoV, and the Venezuelan Equine Encephalitis Virus (VEEV). Cell lines and preclinical research have revealed that NHC is a successful anti-SARS-CoV-2, MERS-CoV, SARS-CoV, and bat-CoVs in related zoonotic classes 2b or 2c. It also effective against resistance due to the mutations to other nucleoside analog blockers in the treatment of a coronavirus [59].
Remdesivir is a nucleotide analog agent that has board spectrum anti-viral activity [60]. It belongs to the class of antihypertensive agents. Diltiazem is a marketed drug that acts by inhibiting voltage-gated Ca2+ channel commonly prescribed to manage angina pectoris and cardiac arrhythmia. The researchers used repurposing of diltiazem as a potential host-directed influenza antagonist due to its so far unknown potential of inducing the IFN anti-viral response, especially type III IFNs [61]. Another in vitro study concluded that remdesivir and a combination with diltiazem could be used as an alternative in the management of the COVID-19 with the help of HAE models [62].
HEK 293T cells
In the year 1977, the human embryonic kidney 293 (HEK 293) cell lines were produced by the transformation of the DNA of the human embryonic kidney cell derived from the sheared Adenovirus5 (Ad5) [63]. For the production of the adenovirus or its related viral vectors, there has been a rise in the importance of 293 cells from the last 20 years. This employs various types of uses in gene therapy. For the recombinant adenoviral vector generation, the HEK 293 cell line and associated cell lines were used as the most prominent host [64]. In addition, these HEK 293 cell cultures can also be used in the cancer cells model for transformation in cellulo and preclinical experiments. HEK-293 cell lines have the following benefits.
(1) An easily transfected human cell line
(2) Readily available
(3) No deposition of collagen is seen
HEK 293T cells are used in various in vitro studies. These cell lines can infect and culturing the SARS-CoV-2 and are used in various types of research work. One of the in vitro studies reported that the human 47D11 monoclonal antibody effective against the SARS-CoV-2 and SARS-CoV in the HEK 293T cells. This antibody targets the communal epitope on both viruses and can serve as therapeutic approaches for treating the SARS-CoV-2 infection [65].
In another study, 26 out of the 29 viral proteins were cloned, labeled, and expressed in HEK 293T cell lines. These were detected physically aligned with the human proteins using affinity-purification mass spectrometry that reported 332 high confidence SARS-CoV-2-human protein-protein interactions (PPI). They found that only 67 druggable human protein and host factors can be targeted by the 69 FDA-licensed medications, pharmaceutical products in clinical trials, and in vivo studies. Identification of various host dependence factors responsible for the viral infections can provide a valuable understanding of the effective molecular targets that can be beneficial in synthesizing wide-spectrum anti-viral drugs in the management of the COVID-19 and other fatal strains of the coronavirus [66].
Calu-3 cells
A Calu-3 2B4 cell culture is among the few human bronchial epithelial cell cultures that form tight junctions in vitro , ideal for modeling the epithelial barrier of the airways used in the pulmonary research work [67]. These cell lines are becoming highly popular in drug delivery and toxicological study. Before spending significant resources on these investigations, the characterization of the epithelium produced in distinct cultural environments is necessary [68]. In the year 1975, Calu-3 cell lines taken from adenocarcinoma epithelium and have serious origin from the proximal bronchial airways of Caucasians at the age of 25 were developed by Fogh [69]. Immuno-staining of desmoplakin shows desmosomes, and E-cadherin shows zonulae adherents in the Calu-3 cell lines. These cell cultures exhibit an mRNA and protein profile belong to the pulmonary epithelial cells [70]. These cell cultures consist of a diverse phenotype that includes secretory and ciliated cells. These differentiates having “tight” junctions, shown with the help of the high Transepithelial Electrical Resistance (TEER) >1000 ohm-cm2. It also has less permeability to paracellular transport markers [71].
The most commonly used Calu-3 has the following benefits:
(a) It is comparable to other cell lines well distinguished, characterized, and derived from sub-mucosal bronchial glands.
(b) At an Air-Liquid Interface (ALI), these cell lines can be cultured easily to form polarized cells compared to other respiratory cell lines. These cells form a pseudo-stratified layer of columnar cells, exhibit an improved ciliogenesis process. It produces a thick mucus gel layer on the surface of epithelial cells and hold superior barrier integrity, typically in the upper airway epithelium.
These cells exhibit the CF transmembrane conductance regulator (cAMP)-dependent chloride secretion. In addition, these cells also have the lung surfactant-specific protein proSP-C and comprise mucin granules [72]. These cell cultures have a system where we can evaluate organic cation transporters-inhaled drug-drug interactions. These all are physiologically appropriate, reproducible, inexpensive, and convenient to work with these cell lines [73]. Specifically, these cells cultured under the ALI medium exhibit a more in vivo like apical surface compared to those cultured in the submerged medium. Therefore, they are more secure from various xenobiotic challenges [74].
Nafamostat Mesylate (NM) is a wide-spectrum serine protease antagonist [75]. Generally, this drug is prescribed in the management of pancreatitis [76], disseminated intravascular coagulation (DIC) [77], and systemic inflammatory response syndrome by inhibition of several factors including thrombin, plasmin, kallikrein, trypsin, and Cl-esterase in the supplementary system [75]. It is also used in the coagulation cascade as it suppresses the factors such as VIIa, Xa, and XIIa [78].
The earlier investigations found that NM antagonized the MERS-CoV protein-initiated membrane fusion via inhibiting transmembrane protease serine2 (TMPRSS2) priming activity. Based on the earlier work, NM was chosen to be the best drug candidate for the COVID-19. Calu-3 cells easily infect SARS-CoV-2. It was found that NM antagonized membrane fusion step at the entry of the virus and inhibited SARS-CoV-2 virus [79].
Another drug candidate for the treatment of COVID-19 was tested in the in vitro study with the help of Calu-3 cell cultures. Suramin is an anti-parasitic drug [80]. This medication is used to manage sleeping sickness in humans due to infection of trypanosomes and onchocerciasis [81]. Further, it is an effective blocker of the reverse transcriptase enzyme (RNA-directed DNA polymerase) found in retroviruses. Scientists revealed that multiplication of SARS-CoV-2 was blocked at the earlier stages, and also drop in the viral load was found in the Calu-3 cell lines treated with the suramin. Also, this drug slows the progression of the disease [82].
Vero Cells
Being a crucial tool for the life sciences, cell cultures that are derived from mammalian tissues are often significant substrates of animal cells for the development of different forms for biological purposes. Vero cell lines are established from the parent source, i.e., from an African green monkey (Cercopithecus aethiops) kidney. Vero cells are one of the utmost frequently utilized mammalian cell cultures [83]. The primary culturing of this tissue was begun on March 27, 1962, by the two scientists Yasumura and Kawikata in Japan. Numerous continuous cell sub-lines were collected afterward passages of a lot of time, and sub-lines were then selected as the standard known as Vero cell line. After their worldwide spread, usage of these cells broadened from virology in research laboratories to medical procedures that include diagnostic procedures of particular diseases in clinics and bacterial toxin testing.
These cell lines are most susceptible to different forms of viruses: a) SV-40 (Simian polyomavirus), b) SARS-CoV and SARS-CoV-2, c) Influenza A and B viruses, d) Arboviruses, e) Adenoviruses, and f). MERS.
It also reported that these cell lines are also susceptible to various toxins of bacteria such as diphtheria toxin and Vero toxins [84]. These cells possess pseudo-diploid karyotype, and they do not form tumors until the cell passage number was not high [85]. The use of animal substrates for the production of the vaccine is needed to be moved from animals and eggs to certain immortal cell cultures, as animal substrates have various concerns that include quality control, stability, and animal ethics. Thus, these cell lines are widely utilized in the cell substrate to produce human vaccines at a large scale [86]. Genetic variations may occur and develop the tumorigenic phenotype of the Vero cells based on the passage number. For instance, high passage numbers (passage 162) indicate genomic instability and tumorigenic potential. Therefore, only a lower passage number of Vero cells has the non-tumorigenic potential that can be used for vaccine development, which might increase concerns as the seed stocks are now declining due to the extensive usage of this cell substrate [87]. These cell lines are the only immortal cell lines approved by the WHO that serve as the cell's substrate for the production of vaccines and other biological purposes to use in humans against different forms of viruses or bacterial toxins. At the beginning of the 1980s, the first use of these Vero cell lines was made by Montagnon and colleagues at the Institute Merieux to develop Inactivated Poliovirus Vaccine (IPV) for human use. For several years, these cells are widely used for oral poliovirus live vaccine production [88]. Subsequently, inactivated rabies vaccine was also manufactured with the usage of Vero cells [89]. An additional key benefit of these cultures for the manufacturing of vaccines is that it is used in the cultivation and infection on micro-carrier beads and cultured in fermenters to facilitate vaccines production. Anton Van Wezel developed this technology, and this can be used for manufacturing polio and rabies virus vaccines [90]. Several vaccines that are effective for chikungunya, dengue fever, Ross River fever, SARS, smallpox, West Nile encephalitis, and influenza have been produced with the help of these cell lines [86]. These cell lines possessed extensive cytopathic effects and plaque formation, which made them an efficient and reproducible direct technique for the demonstration of several viruses and particular neutralizing antibodies [91]. Vero-cells cannot develop type I IFN in response to the virus, the principal reason behind the highly susceptible behavior of these cell lines towards several types of microorganisms [92]. A classical DNA hybridization analysis was already carried out in which researchers found that homozygous deletion of α- and β1-IFN genes were observed in cell lines [93]. There are a variety of commercial cell lines of Vero cells (namely Vero, Vero 76 and Vero E6), but basically all cell lines obtained from the same parent source i.e. African Green Monkey [83].
Literature reported that SARS-CoV-2 infection is highly susceptible to IFN-I pretreatment, although SARS-CoV-2 exhibits almost identical viral replication kinetics in Vero cell culture compared to SARS-CoV. SARS-CoV-2, with type 1 IFN, induces STAT1 phosphorylation and enhances IFN-stimulated genes (ISG) while analyzing the activation of the transcriptional factors and the induction of ISG. On the other side, the original SARS-CoV has no proof of the rise in phosphorylation of STAT1 or ISG protein even though IFN pretreatment is used. The findings together describe significant variations in IFN-I pretreatment responses of SARS-CoV in contrast to SARS-CoV-2. These results can benefit in finding the novel 'therapeutics' for the COVID-19 and help develop the in vivo models [94].
Therapeutic Agents Using in vitro Models Especially Vero and Vero Derived Cell Lines
Remdesivir
American pharmaceutical industry Gilead Sciences launched a drug Remdesivir that is a prodrug of a 1’-cyano-substituted nucleotide derivative shown potential effect during Ebola virus spread owing to its low 50% effective concentrations (EC50) along with its selectivity to host polymerase in the treatment of the Ebola virus [95]. The compound has shown a wide-spectrum anti-viral potential. It is widely used in the management of the members of several virus families, namely filoviruses (e.g., Ebola virus), paramyxoviruses (e.g., Nipah virus), and coronaviruses (e.g., SARS-CoV and MERS-CoV). For RNA viruses such as SARS-CoV-2, multiplication depends on the viral RNA-dependent RNA polymerase (RdRp), which presents an optimal target due to its important role in RNA synthesis [96]. A recent cell line study showed that remdesivir has potency and has very few adverse effects in the SARS-CoV-2 infection in Vero E6 cell lines. The reported EC50 value of this drug was 23.15 µM against this infection [97]. Remdesivir is an adenosine analog that is resistant to exonuclease. It is intracellularly changed into active metabolite nucleoside triphosphates. It helps to efficiently inhibit the RNA chain elongation by terminating the enzyme RNA polymerase. However, this drug cannot be absorbed by viral exonuclease (nsp14) having proofreading activity [98]. So, this is a promising drug amongst all drugs to manage the SARS-CoV-2 virus [96].
Lopinavir
Lopinavir is a potent protease blocker and is prescribed to manage HIV type 1 (HIV-1), a crucial enzyme used to produce mature infectious viruses. It works by preventing HIV-1 maturation, thus blocking infectivity [99]. Therefore, the mechanism behind the anti-viral activity of lopinavir is to prevent consequent susceptible cell infections. It also does not show an effect on cells that have integrated viral DNA. Lopinavir has a higher in vitro activity against both wild-type and mutant HIV-1 proteases than ritonavir (an inhibitor of the cytochrome P450 3A isoenzyme). But, its efficacy is critically reduced due to the poor bioavailability of the pre-systemic metabolism in vivo model. Lopinavir is used in combination with a reduced dosage of ritonavir that considerably improves plasma concentrations of the drug and helps achieve high and consistent levels of lopinavir [100]. Both protease inhibitors prevent viral nucleic acid multiplication by blocking 3CLpro [101]. In the cell line, investigations of lopinavir as an anti-SARS-CoV-2 in the Vero E6 cell lines were found to be effective.
In addition, co-administration of lopinavir with the other effective drugs against the treatment of COVID-19. It enhances synergism and decreases the inhibitory concentration of lopinavir [97]. Therefore, lopinavir warrants further study for possible benefits in the treatment of COVID-19 shown in Table 2.
Homorringtonine
Homoharringtonine (HHT) is an alkaloid obtained from Cephalotoxus fortunei with anti-leukemic activity and had been the drug of choice for treating patients suffering from acute and chronic myeloid leukemia. The main mechanism by which HHT works is the interruption of the translation process, which is dependent on dose and time as it binds to the ribosome and prevents polypeptide chain elongation [102]. In 2012, Omacetaxine, a semisynthetic derivative of HHT, was licensed by the FDA to manage chronic myeloid leukemias. According to past investigations, HHT has shown anti-viral action and can be used to manage herpesviruses, coronaviruses, and rhabdoviruses [103]. HHT binds to the 80S ribosome and blocked viral protein translation machinery via interrupting chain elongation [104]. In a recent investigation, it was observed that HHT is effective against SARS-CoV-2 infection with EC50 2.10 µM in the cell cultures of Vero E6 [97]. Altogether, as a phytoconstituents, HHT is extensively distributed however, its potent anti-viral action in a plethora of viruses requires more exploration.
Emetine hydrochloride
Emetine is an alkaloid obtained from the Psychotria ipecacuanha Stokes (Rubiaceae). This herbal plant is called Cephaelis ipecacuanha. It is among the major active constituents in ipecac syrup marketed as an emetic and has been widely utilized in herbal medication as an anti-protozoan agent. The mode of action by which it works is that it blocked both ribosomal and mitochondrial protein translation machinery synthesis and hinders the synthesis and functions of nucleic acids. Emetine is used in the management of both intestinal and extraintestinal amoebiasis. It helps in amebic dysentery caused by the infection of Entamoeba histolytica, an anaerobic parasitic protozoan [105]. Emetine works as an anti-viral action. According to the past findings, emetine interferes with the viral protein synthesis by inhibiting the 40S ribosomal protein S14 in cells of the host. It has been reported that emetine inhibits HIV reverse transcriptase enzyme, block viral polymerases [106]. In the studies related to the COVID-19 treatment, emetine has shown positive results. In the cell line study, emetine inhibits the SARS-CoV-2 viral multiplication in the Vero E6 cells [97]. Overall, emetine has an anti-viral action, which indicated that emetine is a potential remedy in managing the SARS-CoV-2.
Ivermectin
Ivermectin is a macrocyclic lactone structurally similar to its naturally occurring fermentation product, avermectin B1, obtained from an actinomycete, Streptomyces avermitilis. Ivermectin is an anti-parasitic agent and mainly active against two main phyla of the animal kingdom- a) the Nemathelminthes or nematodes (roundworms) and b) the arthropod (insects, ticks, and mites). The mode of action of ivermectin is the same as avermectin B1 [107]. They paralyze body-wall muscle in nematodes and arthropods via disrupting gamma-aminobutyric acid (GABA)-mediated chloride ion conductance of nerve signals. It has been extensively prescribed to manage the patients having the infection caused by nematode Onchocerca volvulus, which is the main reason for blindness in natives of some tropical regions [108]. Subsequently, the latest research showed that ivermectin has an effective role in the SARS-CoV-2 infection in the Vero/hSLAM cell lines, and half inhibitory concentration (IC50) was found to be ~2 μM [109]. The possible anti-viral mechanism of ivermectin acts by inhibition of IMPα/β1 responsible for the nuclear import proteins of the virus [110] shown in Table 2. Overall, this drug requires further investigation for its efficacy in human to manage the SARS-CoV-2 virus.
Chloroquine/Hydroxychloroquine
Chloroquine and its less toxic derivative hydroxychloroquine are two inexpensive drugs that have been used traditionally as a wide-spectrum therapy for malaria and autoimmune disease [111]. The underlying mechanism of chloroquine and hydroxychloroquine as an anti-viral agent against coronavirus is still unclear. Earlier investigations have suggested that both these drugs block virus infection from entering into the host via inhibition of glycosylation of host cell receptors and proteolytic processing by increasing endosomal pH. Moreover, they improve immunity via reducing the number of cytokines that inhibit the autophagy and lysosomal action in the cells [112, 113]. The latest investigation suggested that chloroquine worked at entry and post-entry stages of the SARS-CoV-2 virus in Vero E6 cell lines, and EC50 was 1.13 μM and half-cytotoxic concentration (CC50) was less than 100 μM [114]. Hydroxychloroquine also showed its potential in the management of COVID-19 in Vero E6 cells [115]. Therefore, it can be reasonably speculated that these are potential drugs for SARS-CoV-2 infection. So, its effective against COVID-19 deserves further study for its efficacy in the human.
Nelfinavir
Nelfinavir is a nonpeptidic, specific, and HIV protease competitive antagonist. It is the main enzyme required for post-translational modifications of HIV propeptides [116]. Nelfinavir has a good safety profile and potent drug in the management of HIV-1 and HIV-2 viruses. Nelfinavir was developed by the private pharmaceutical industry and gained popularity for the management of AIDS in combination with other antiretroviral agents [117]. This drug has been investigated due to its off-target anticancer mechanism [118]. Nelfinavir is also tested for the treatment of COVID-19 in Vero E6 cell cultures in recent investigations. Findings suggested that this protease inhibitor significantly inhibits cell fusion of the viral envelope caused by spike (S) glycoprotein, a key factor in virus infectivity [119-121]. in vitro studies, nelfinavir has shown high potency against SARS-CoV-2 infection, requiring further exploration for managing COVID-19.
Indomethacin
Indomethacin categorizes in the class as a non-steroidal anti-inflammatory drug (NSAIDs) are extensively prescribed painkillers in the treatment of headache and many of the primary headache disorders [122]. It has a potent inhibitory action on the synthesis of prostaglandins that has a crucial role in the anti-inflammatory response. The production of prostaglandins is blocked as it inhibits cyclooxygenases (COX) 1 and 2 enzymes and is important for most NSAIDs. Indomethacin is prescribed to manage arthritis, fever, several headache syndromes, and dysmenorrhea [123]. Past investigations showed that indomethacin has potency in treating the SARS-CoV virus. In the latest experiments where indomethacin has shown its potency in treating the SARS-CoV-2 virus in the Vero E6 cells. The molecular mechanism underlying the anti-viral activity of indomethacin in the management of the SARS-CoV-2 virus is not fully known and requires further investigation. Results suggested that the possible mechanism of indomethacin as an anti-viral agent may be due to the reduction in the IL-6 and inhibit RNA synthesis [124-126] mentioned in Table 2. Overall, indomethacin is a potent inhibitor of SARS-CoV-2 infection and warrants further exploration.
Merimepodib
Merimepodib is an orally bioavailable, potent, selective, reversible, and uncompetitive antagonist of inosine-5'-monophosphate dehydrogenase (IMPDH) [127]. A crucial component catalyzes the rate-limiting step in the de novo synthesis of the purine nucleotides biosynthesis pathway. Thus, blocking IMPDH could reduce the intracellular guanosine triphosphate (GTP) that is mandatory for the transcription process at the time of viral replication. Merimepodib was marketed for the managing of the hepatitis C virus (HCV) [128]. Literature reveals that merimepodib has in vitro anti-viral activity against Ebola, Lassa, and Zika virus [129]. The in vitro investigations suggested that merimepodib work as an anti-coronavirus agent against SARS-CoV-2 virus in the Vero E6 cell lines found to be effective and 50% tissue culture, infectious dose (TCID50) was 3.3 μM. It is probably due to its IMPDH suppression, which is responsible for guanosine depletion when replication by viral polymerase [130]. Consequently, merimepodib may be a promising COVID-19 therapy alternative that should be further explored for efficacy in humans.
Scutellaria baicalensis
Scutellaria baicalensis (S. baicalensis), also known as Chinese skullcap or Huangqin, is amongst the utmost important medicinal herb prescribed in Chinese herbal medicine and is formally mentioned in the Chinese Pharmacopoeia. This herb possesses a plethora of biological and pharmacological actions, including anti-inflammatory, anticancer, anti-viral, anti-bacterial, anti-hypertensive, and sedative effects. This herb comprises several flavonoids [131]. Baicalin, baicalein, wogonin, and oroxylin A are the major active constituents found in S. baicalensis (Georgi), are flavone derivatives containing a phenylbenzopyrone moiety [132]. Various studies are ongoing to find the treatment options for the COVID-19. One of the study ethanolic extracts of S. baicalensis (Georgi) and baicalein, one of the flavonoids of this herbal drug, exhibits anti-coronavirus activity as they inhibit the multiplication of SARS-CoV-2 virus in Vero E6 cell cultures. The proposed mechanism behind its anti-viral activity is due to the inhibition of 3CLpro and prevents viral nucleic acid multiplication [133]. Taken together, the results of this investigation provide evidence that S. baicalensis Georgi and baicalein may serve as a viable treatment alternative for COVID-19.
Gemcitabine
Gemcitabine is a novel pyrimidine nucleoside derivative of cytarabine (cytosine arabinoside) in which two fluorine atoms have been introduced into deoxyribofuranosyl ring widely used as a standard chemotherapeutic agent [134]. Gemcitabine is different from other anticancer drugs due to its comparatively few adverse effects (typically mild fatigue and modest bone-marrow suppression). Its wide range of activity against different cancers and potency inhibit deoxynucleotide metabolism at clinically effective doses [135]. This drug also possesses anti-viral action in managing various RNA viruses, including enterovirus 71, human rhinoviruses (HRVs), MERS-CoV, SARS-CoV, and coxsackievirus B3. The anti-viral mechanism of gemcitabine hinders the salvage pathway of pyrimidine synthesis and improves innate immunity [136]. Recently, the study reported that gemcitabine has anti-viral action against SARS-CoV-2 infection (EC50= 1.24 µM) in Vero E6 cell cultures [137]. These results demonstrated that gemcitabine may be the alternative option in the COVID-19 therapy but requires preclinical and clinical studies to evaluate the efficacy.
Carmofur
Carmofur (HCFU; 1-Hexylcarbamoyl-5-fluorouracil, Mifurol) is a fluorinated pyrimidine derivate of 5-fluorouracil (5-FU) has an anticancer action, is one of the key drug prescribed to manage individuals suffering from a variety of malignancies [138]. Carmofur is orally bioavailable, used as a solo compound. It is used as adjuvant therapy in cervical carcinoma, breast, colorectal cancer, and gastrointestinal carcinomas. Carmofur is an orally administered prodrug that metabolized intracellularly to active form 5-FU. It helps to inhibits thymidylate synthetase, which is responsible for catalyzing the deoxyuridine monophosphate (dUMP) into deoxythymidine monophosphate (dTMP). Thus, it will inhibit tumor proliferation [139]. HCFU drug is also a potent acid human ceramidase inhibitor marketed as an adjuvant chemotherapeutic agent in Japan since 1981 [140]. In numerous RNA and DNA viruses, proteases have a crucial role in the viral multiplication process. Thus, proteases are frequently used as therapeutic targets during the development of anti-coronavirus drugs [141]. A recent in silico study showed with the help of the X-ray crystallography structure of SARS-CoV-2 main protease (Mpro) forms a complex with HCFU. Moreover, in vitro evaluation of carmofur reveals that this drug inhibits viral replication in Vero E6 cell culture (EC50 = 24.30 μM) [142]. Therefore, carmofur serves as a potential lead molecule that can be utilized to manage COVID-19.
Arbidol
The anti-viral medicine arbidol (ARB) is a derivative of indole used in Russia and China in 1993 and 2006, respectively to prevent and manage influenza A, B, and C viruses [143]. In preclinical in cellulo studies, ARB has potential anti-viral action against several numbers of RNA or DNA viruses [144]. The mechanism behind the anti-viral action of this molecule acts on important steps of host-virus interactions. It may directly act on the interaction of membrane fusion with the chief players of the primary steps of virus entry and prevents multiplication. Consequently, ARB may also have the potential role to serve as a host-targeting agent (HTA) [145]. Recently, ARB also tested for the SARS-CoV-2 virus treatment, and positive results were seen in Vero E6 cells. ARB inhibits the SARS-CoV-2 virus as it interferes with attachment and intracellular vesicle trafficking [146]. Therefore, results suggested that ARB may be a promising COVID-19 therapy alternative that should be further explored for efficacy in clinical trials.
Table 2 Summary of the possible drugs against SARS-CoV-2 infection.
|
S. No. |
Drug |
Pharmacological Activity |
Subjects |
EC50 |
IC50 |
CC50 |
Mechanism of Action |
References |
|
1. |
Remdesivir |
Adenosine analog |
Vero E6 cells |
23.15 |
- |
> 100 |
Inhibits RdRp |
[96, 97] |
|
2. |
Lopinavir |
Protease inhibitor |
Vero E6 cells |
26.63 |
- |
49.75 |
Inhibits 3CLpro |
[97, 101] |
|
3. |
Homorringtonine |
Anticancer |
Vero E6 cells |
2.55 |
- |
59.75 |
Inhibits protein synthesis |
[97, 104] |
|
4. |
Emetine |
Anti- protozoal |
Vero E6 cells |
0.46 |
- |
56.46 |
Inhibits protein synthesis |
[97, 105] |
|
5. |
Ivermectin |
Anti-parasitic |
Vero/hSLAM cells |
- |
2 |
- |
Inhibits IMPα/β1 responsible for nuclear import of proteins of the virus |
[109, 110] |
|
6. |
Chloroquine/ Hydroxychloroquine |
Anti-malarial |
Vero E6 cells |
1.13 / |
- |
> 100 |
Inhibits endosomal acidification fusion and improves immunity |
[114, 115], |
|
7. |
Nelfinavir |
Protease antagonist |
VeroE6/ |
1.13 |
- |
24.32 |
Inhibits cell fusion mediated by SARS-CoV‐2 spike (S) glycoprotein |
[120, 121] |
|
8. |
Indomethacin |
Cyclooxygenases inhibitor |
Vero E6 cells |
1 |
- |
- |
Inhibits RNA synthesis, reduces IL-6 production |
[125, 126] |
|
9. |
Merimepodib |
IMPDH inhibitor |
Vero cells |
- |
- |
- |
Reduction in the GTP involved in the viral replication |
[130] |
|
10. |
Scutellaria baicalensis |
Anti-viral, anti-hypertensive, anti-bacterial, anticancer. |
Vero cells |
- |
8.5 μg/ml (extract) |
- |
Inhibits 3CLpro |
[133] |
|
11. |
Gemcitabine |
Anticancer |
Vero E6 cells |
1.24 |
- |
>40 |
Inhibits pyrimidine biosynthesis and improves innate immunity |
[136, 137] |
|
12. |
Carmofur |
Anti-cancer |
Vero E6 cells |
24.30 |
- |
133.4 |
Inhibits SARS-CoV-2 main protease (Mpro) |
[142] |
|
13. |
Arbidol |
Anti-influenza |
Vero E6 cells |
4.11 |
- |
31.79 |
Interferes viral binding |
[146] |
CONCLUDING REMARKS
In conclusion, these cell lines such as Vero, Calu-3, A549, Huh-7, and Caco-2 make accessible to the national and international public health, academia, and pharmaceutical industries for fundamental studies, diagnostic purposes, evaluation of anti-viral agents, and manufacturing of vaccine. We look forward to the collaboration of all researchers worldwide to expedite countermeasure development and testing for SARS-CoV-2. It could assist a good understanding of the pathophysiology of this novel SARS-CoV-2 infection. Moreover, these cell lines can be used as effective drug development candidates to manage the recent and upcoming potential of the SARS-CoV-2 virus. It is also used to control the further spread of this pandemic. However, preclinical and clinical studies are equivalently crucial for effective drug development in managing the COVID-19.
CONSENT FOR PUBLICATION
Not applicable.
CONFLICT OF INTEREST
The author confirms that this chapter contents have no conflict of interest.
ACKNOWLEDGEMENT
Declared none.
REFERENCES
|
[1] |
Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges 2020; Vol. 55: 105924. |
|
[2] |
Li X, Geng M, Peng Y, Meng L, Lu S. Molecular immune pathogenesis and diagnosis of COVID-19 J Pharmaceut Analysis 2020. |
|
[3] |
Chen Y, Liu Q, Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol 2020; 92(4): 418-23.[http://dx.doi.org/10.1002/jmv.25681] [PMID: 31967327] |
|
[4] |
Tortorici MA, Veesler D. Structural insights into coronavirus entry. Advances in Virus Research 201993-116. |
|
[5] |
Wu A, Peng Y, Huang B, et al. Genome composition and divergence of the novel coronavirus (2019-ncov) originating in China. Cell Host Microbe 2020; 27(3): 325-8.[http://dx.doi.org/10.1016/j.chom.2020.02.001] [PMID: 32035028] |
|
[6] |
Zhou P, Yang X-L, Wang X-G, Hu B, Zhang L, Zhang W. Discovery of a novel coronavirus associated with the recent pneumonia outbreak in humans and its potential bat origin. Nature 2020; 579(7798): 270-3.[http://dx.doi.org/10.1038/s41586-020-2012-7] |
|
[7] |
Velavan TP, Meyer CG. The COVID-19 epidemic. Tropical Medicine & International Health 2020; 25(3): 278.[http://dx.doi.org/10.1101/2020] |
|
[8] |
Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395(10224): 565-74.[http://dx.doi.org/10.1016/S0140-6736(20)30251-8] [PMID: 32007145] |
|
[9] |
Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395(10223): 507-13.[http://dx.doi.org/10.1016/S0140-6736(20)30211-7] [PMID: 32007143] |
|
[10] |
Gómez-Lechón MJ, Donato MT, Castell JV, Jover R. Human hepatocytes as a tool for studying toxicity and drug metabolism. Curr Drug Metab 2003; 4(4): 292-312.[http://dx.doi.org/10.2174/1389200033489424] [PMID: 12871046] |
|
[11] |
MacDonald C. Development of new cell lines for animal cell biotechnology. Crit Rev Biotechnol 1990; 10(2): 155-78.http://www.ncbi.nlm.nih.gov/pubmed/2202521[http://dx.doi.org/10.3109/07388559009068265] [PMID: 2202521] |
|
[12] |
Birch JR. Culture of animal cells: A manual of basic technique: By R. I. Freshney. J Chem Technol Biotechnol 2007; 45(4): 330.[http://dx.doi.org/10.1002/jctb.280450414] |
|
[13] |
Hudu SA, Alshrari AS, Syahida A, Sekawi Z. Cell Culture, Technology: Enhancing the Culture of Diagnosing Human Diseases. J Clin Diagn Res 2016; 10(3): DE01-5.[http://dx.doi.org/10.7860/JCDR/2016/15837.7460] [PMID: 27134874] |
|
[14] |
Gillim-Ross L, Taylor J, Scholl DR, Ridenour J, Masters PS, Wentworth DE. Discovery of novel human and animal cells infected by the severe acute respiratory syndrome coronavirus by replication-specific multiplex reverse transcription-PCR. J Clin Microbiol 2004; 42(7): 3196-206. http://www.ncbi.nlm.nih.gov/pubmed/15243082[http://dx.doi.org/10.1128/JCM.42.7.3196-3206.2004] [PMID: 15243082] |
|
[15] |
Barenfanger J, Drake C, Mueller T, Troutt T, O’Brien J, Guttman K. R-Mix cells are faster, at least as sensitive and marginally more costly than conventional cell lines for the detection of respiratory viruses. J Clin Virol 2001; 22(1): 101-10. https://linkinghub.elsevier.com/ret rieve/pii/S1386653201001718 [Internet].[http://dx.doi.org/10.1016/S1386-6532(01)00171-8] [PMID: 11418357] |
|
[16] |
Zucco F, Batto A, Bises G. An inter-laboratory study to evaluate the effects of medium composition on the differentiation and barrier function of Caco-2 cell lines. JC-A 2005. Available from: journals.sagepub.com journals.sagepub.com [Internet]. [cited 2020 Apr 29].[http://dx.doi.org/10.1177/026119290503300618] |
|
[17] |
Artursson P. Epithelial transport of drugs in cell culture. I: A model for studying the passive diffusion of drugs over intestinal absorptive (Caco-2) cells. J Pharm Sci 1990; 79(6): 476-82.[http://dx.doi.org/10.1002/jps.2600790604] [PMID: 1975619] |
|
[18] |
Yi W, Akoh CC, Fischer J, Krewer G. Absorption of anthocyanins from blueberry extracts by caco-2 human intestinal cell monolayers. J Agric Food Chem 2006; 54(15): 5651-8.[http://dx.doi.org/10.1021/jf0531959] [PMID: 16848559] |
|
[19] |
Chantret I, Rodolosse A, Barbat A, Dussaulx E, Brot-Laroche É, Zweibaum A. Differential expression of sucrase-isomaltase in clones isolated from early and late passages of the cell line Caco-2: evidence for glucose-dependent negative regulation. J Cell Sci 1994; 107(Pt 1): 213-5. |
|
[20] |
Chiu E, Chow Y, Sun H, Chow EC, Liu S, Du Y. The Caco-2 cell monolayer: Usefulness and limitations. Artic Expert Opin Drug Metab Toxicol [Internet] 2008; 4(4): 395-411.[http://dx.doi.org/] [PMID: ] [cited 2020 Apr 29] Available from: https://www.researchgate.net/publication/5420246 |
|
[21] |
De Meyer S, Bojkova D, Cinatl J, Van Damme E, Meng CB, Van Loock M. Lack of anti-viral activity of darunavir against SARS-CoV-2. Int J Infect Dis 2020; 97: 7-10.[http://dx.doi.org/10.1101/2020.04.03.20052548] |
|
[22] |
Nault JC, Galle PR, Marquardt JU. The role of molecular enrichment on future therapies in hepatocellular carcinoma. J Hepatol 2018; 69(1): 237-47.[http://dx.doi.org/10.1016/j.jhep.2018.02.016] |
|
[23] |
Finn RS, Aleshin A, Dering J, et al. Molecular subtype and response to dasatinib, an Src/Abl small molecule kinase inhibitor, in hepatocellular carcinoma cell lines in vitro . Hepatology 2013; 57(5): 1838-46. [Internet].[http://dx.doi.org/10.1002/hep.26223] [PMID: 23299860] |
|
[24] |
Dzieran J, Fabian J, Feng T, Coulouarn C, Ilkavets I, Kyselova A. Comparative Analysis of TGF-β/Smad Signaling Dependent Cytostasis in Human Hepatocellular Carcinoma Cell Lines. PLoS One [Internet] 2013; 8(8): e72252.[http://dx.doi.org/10.1371/journal.pone.0072252] |
|
[25] |
Nakabayashi H, Taketa K, Miyano K, Yamane T, Sato J. Growth of human hepatoma cells lines with differentiated functions in chemically defined medium. Cancer Res 1982; 42(9): 3858-63.[PMID: 6286115] |
|
[26] |
Lohmann V, Körner F, Koch JO, Herian U, Theilmann L, Bartenschlager R. Replication of subgenomic hepatitis C virus RNAs in a hepatoma cell line. Science 1999; 285(5424): 110-3.[http://dx.doi.org/10.1126/science.285.5424.110] |
|
[27] |
Ding Y, Zeng L, Li R, et al. The Chinese prescription lianhuaqingwen capsule exerts anti-influenza activity through the inhibition of viral propagation and impacts immune function. BMC Complement Altern Med 2017; 17(1): 130.[http://dx.doi.org/10.1186/s12906-017-1585-7] [PMID: 28235408] |
|
[28] |
Runfeng L, Yunlong H, Jicheng H, et al. Lianhuaqingwen exerts anti-viral and anti-inflammatory activity against novel coronavirus (SARS-CoV-2). Pharmacol Res 2020; 156: 104761.[http://dx.doi.org/10.1016/j.phrs.2020.104761] [PMID: 32205232] |
|
[29] |
Wang X, Xu W, Hu G, Xia S, Sun Z, Liu Z. SARS-CoV-2 infects T lymphocytes through its spike protein-mediated membrane fusion 20201-3. |
|
[30] |
Liu C, Yang Y, Gao Y, Shen C, Ju B, Liu C. Viral architecture of SARS-CoV-2 with post-fusion spike revealed by Cryo-EM. Structure 2020; 28(11): 1218-1224.e4.[http://dx.doi.org/10.1016/j.str.2020.10.001] |
|
[31] |
Ryan RM, Mineo-Kuhn MM, Kramer CM, Finkelstein JN. Growth factors alter neonatal type II alveolar epithelial cell proliferation. Am J Physiol 1994; 266(1 Pt 1): L17-22. http://www.ncbi.nlm.nih.gov/pubmed/8304465 [Internet].[PMID: 8304465] |
|
[32] |
Foster KA, Oster CG, Mayer MM, Avery ML, Audus KL. Characterization of the A549 cell line as a type II pulmonary epithelial cell model for drug metabolism. Exp Cell Res 1998; 243(2): 359-66.[http://dx.doi.org/10.1006/excr.1998.4172] [PMID: 9743595] |
|
[33] |
Corbière V, Dirix V, Norrenberg S, Cappello M, Remmelink M, Mascart F. Phenotypic characteristics of human type II alveolar epithelial cells suitable for antigen presentation to T lymphocytes. Respir Res 2011; 12(1): 15.http://respiratory-research.biomedcentral.com/articles/10.1186/1465-9921-12-15 [Internet].[http://dx.doi.org/10.1186/1465-9921-12-15] [PMID: 21261956] |
|
[34] |
Lieber M, Smith B, Szakal A, Nelson-Rees W, Todaro G. A continuous tumor-cell line from a human lung carcinoma with properties of type II alveolar epithelial cells. Int J Cancer 1976; 17(1): 62-70.[http://dx.doi.org/10.1002/ijc.2910170110] [PMID: 175022] |
|
[35] |
Jiang RD, Shen H, Piao YJ. The morphometrical analysis on the ultrastructure of A549 cells. Rom J Morphol Embryol 2010; 51(4): 663-7.[PMID: 21103623] |
|
[36] |
Blanco-Melo D, Nilsson-Payant BE, Liu W-C, Møller R, Panis M, Sachs D. SARS-CoV-2 launches a unique transcriptional signature from in vitro, ex vivo, and in vivo systems. bioRxiv 2020.[http://dx.doi.org/10.1101/2020.03.24.004655] |
|
[37] |
Busti AJ, Hall RG, Margolis DM. Atazanavir for the treatment of human immunodeficiency virus infection. Pharmacotherapy 2004; 24(12): 1732-47. http://doi.wiley.com/10.1592/phco.24.17.1732. 52347[http://dx.doi.org/10.1592/phco.24.17.1732.52347] [PMID: 15585441] |
|
[38] |
Fintelman-Rodrigues N, Sacramento CQ, Ribeiro Lima C, Souza da Silva F, Ferreira AC, Mattos M. Atazanavir inhibits SARS-CoV-2 replication and pro-inflammatory cytokine production. Antimicrob Agents Chemother 2020; 64(10): e00825-20.[http://dx.doi.org/10.1101/2020.04.04.020925] |
|
[39] |
Barker N, van Es JH, Kuipers J, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature 2007; 449(7165): 1003-7.[http://dx.doi.org/10.1038/nature06196] [PMID: 17934449] |
|
[40] |
Wright NA. Epithelial stem cell repertoire in the gut: clues to the origin of cell lineages, proliferative units and cancer. Int J Exp Pathol 2000; 81(2): 117-43.[http://dx.doi.org/10.1046/j.1365-2613.2000.00146.x] [PMID: 10762441] |
|
[41] |
Cheng H, Leblond CP. Origin, differentiation and renewal of the four main epithelial cell types in the mouse small intestine. V. Unitarian Theory of the origin of the four epithelial cell types. Am J Anat 1974; 141(4): 537-61.http://doi.wiley.com/10.1002/aja.1001410407 [Internet].[http://dx.doi.org/10.1002/aja.1001410407] [PMID: 4440635] |
|
[42] |
Sato T, Vries RG, Snippert HJ, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 2009; 459(7244): 262-5.[http://dx.doi.org/10.1038/nature07935] [PMID: 19329995] |
|
[43] |
Y Sasai. Next-generation regenerative medicine: organogenesis from stem cells in 3D culture. Cell stem cell 2013; 12(5): 520-30.[http://dx.doi.org/10.1016/j.stem.2013.04.009] |
|
[44] |
van de Wetering M, Francies HE, Francis JM, et al. Prospective derivation of a living organoid biobank of colorectal cancer patients. Cell 2015; 161(4): 933-45.[http://dx.doi.org/10.1016/j.cell.2015.03.053] [PMID: 25957691] |
|
[45] |
Okita K, Ichisaka T, Yamanaka S. Generation of germline-competent induced pluripotent stem cells. Nature 2007; 448(7151): 313-7. http://www.jwildlifedis.org/doi/10.7589/0090-3558-37.4.755 [Internet].[http://dx.doi.org/10.1038/nature05934] [PMID: 17554338] |
|
[46] |
O’Brien JA, Lahue BJ, Caro JJ, Davidson DM. The emerging infectious challenge of clostridium difficile-associated disease in Massachusetts hospitals: clinical and economic consequences. Infect Control Hosp Epidemiol 2007; 28(11): 1219-27.[http://dx.doi.org/10.1017/S0195941700026072] [PMID: 17926270] |
|
[47] |
Engevik MA, Engevik KA, Yacyshyn MB, et al. Human Clostridium difficile infection: inhibition of NHE3 and microbiota profile. Am J Physiol Gastrointest Liver Physiol 2015; 308(6): G497-509.[http://dx.doi.org/10.1152/ajpgi.00090.2014] [PMID: 25552580] |
|
[48] |
Gu J, Han B, Wang J. COVID-19: gastrointestinal manifestations and potential fecal–oral transmission. Gastroenterology 2020; 158(6): 1518-9. |
|
[49] |
Wang W, Xu Y, Gao R, Lu R, Han K, Wu G. Detection of SARS-CoV-2 in different types of clinical specimens. Jama 323(18): 1843-4. |
|
[50] |
Ettayebi K, Crawford S. Replication of human noroviruses in stem cell–derived human enteroids. 2016. [cited 2020 May 6]; Available from: https://science.sciencemag.org/content/353/ 6306/1387.short |
|
[51] |
Beumer J, Artegiani B, Post Y, Reimann F. Enteroendocrine cells switch hormone expression along the crypt-to-villus BMP signalling gradient. [cited 2020 May 6]; Available from: https://www.nature.com/articles/s41556-018-0143-y |
|
[52] |
Lamers MM, Beumer J, van der Vaart J, Knoops K, Puschhof J, Breugem TI. SARS-CoV-2 productively infects human gut enterocytes. Science 2020.[http://dx.doi.org/doi/10.1126/science.abc1669] |
|
[53] |
Fulcher ML, Randell SH. Human nasal and tracheo-bronchial respiratory epithelial cell culture. Methods Mol Biol 2013; 945: 109-21.[http://dx.doi.org/10.1007/978-1-62703-125-7_8] [PMID: 23097104] |
|
[54] |
Fulcher ML, Gabriel S, Burns KA, Yankaskas JR, Randell SH. Well-differentiated human airway epithelial cell cultures. Methods Mol Med 2005; 107: 183-206.[http://dx.doi.org/10.1385/1-59259-861-7:183] [PMID: 15492373] |
|
[55] |
Gruenert DC, Finkbeiner WE, Widdicombe JH. Culture and transformation of human airway epithelial cells. Am J Physiol 1995; 268(3 Pt 1): L347-60.[http://dx.doi.org/10.1152/ajplung.1995.268.3.L347] [PMID: 7900815] |
|
[56] |
Forbes I. Human airway epithelial cell lines for in vitro drug transport and metabolism studies. Pharm Sci Technol Today 2000; 3(1): 18-27. https://linkinghub.elsevier.com/retrieve/pii/S146153479900 231X[http://dx.doi.org/10.1016/S1461-5347(99)00231-X] [PMID: 10637597] |
|
[57] |
Yankaskas JR, Cotton CU, Knowles MR, Gatzy JT, Boucher RC. Culture of human nasal epithelial cells on collagen matrix supports. A comparison of bioelectric properties of normal and cystic fibrosis epithelia. Am Rev Respir Dis 1985; 132(6): 1281-7.[PMID: 4073668] |
|
[58] |
Sheahan T, Sims A. Broad-spectrum anti-viral GS-5734 inhibits both epidemic and zoonotic coronaviruses. RG-S translational, 2017 undefined RG-S translational, 2017 undefined. Broad-spectrum anti-viral GS-5734 inhibits both epidemic and zoonotic coronaviruses. stm.sciencemag.org [Internet]. [cited 2020 May 13]; Available from: https://stm.sciencemag.org |
|
[59] |
Sheahan TP, Sims AC, Zhou S, Hill C, Leist SR, Schaefer A. An orally bioavailable broadspectrum anti-viral inhibits SARS-CoV-2 and multiple endemic, epidemic and bat coronavirus. Science (80-) 2020.https://www.biorxiv.org/content/10.1101/2020.03.19.997890v1 |
|
[60] |
PubChem [Internet]. [cited 2020 May 13]. Available from: https://pubchem.ncbi.nlm.nih.gov /#query=remdesivir |
|
[61] |
Diltiazem | C22H26N2O4S - PubChem [Internet]. [cited 2020 May 13]. Available from: https://pubchem.ncbi.nlm.nih.gov/compound/39186 |
|
[62] |
Pizzorno A, Padey B, Julien T, Trouillet-Assant S, Traversier A, Errazuriz-Cerda E. Characterization and treatment of SARS-CoV-2 in nasal and bronchial human airwayepithelia bioRxiv 2020.http://biorxiv.org/content/early/2020/04/02/2020.03.31.01788 |
|
[63] |
Graham FL, Smiley J, Russell WC, Nairn R. Characteristics of a human cell line transformed by DNA from human adenovirus type 5. J Gen Virol 1977; 36(1): 59-74. [Internet]. https://www.microbiologyresearch.org /content/journal/jgv/10.1099/0022-1317-36-1-59[http://dx.doi.org/10.1099/0022-1317-36-1-59] [PMID: 886304] |
|
[64] |
Berkner KL. Development of adenovirus vectors for the expression of heterologous genes. Biotechniques 2020; 6(7): 29-616.[PMID: 3078719] |
|
[65] |
Wang C, Li W, Drabek D, et al. A human monoclonal antibody blocking SARS-CoV-2 infection. Nat Commun 2020; 11(1): 2251.http://www.nature.com/articles/s41467-020-16256-y [Internet].[http://dx.doi.org/10.1038/s41467-020-16256-y] [PMID: 32366817] |
|
[66] |
Gordon DE, Jang GM, Bouhaddou M, Xu J, Obernier K. O Meara MJ, et al. A SARS-CoV-2-Human Protein-Protein Interaction Map Reveals Drug Targets and Potential Drug-Repurposing bioRxiv http://biorxiv.org/content/early/2020/03/27/2020.03.22.002386 |
|
[67] |
Florea BI, Cassara ML, Junginger HE, Borchard G. Drug transport and metabolism characteristics of the human airway epithelial cell line Calu-3. J Control Release 2003131-8.[http://dx.doi.org/10.1016/S0168-3659(02)00356-5] |
|
[68] |
Forbes B, and CE-E journal of pharmaceutics, 2005 undefined. Human respiratory epithelial cell culture for drug delivery applications. Elsevier [Internet]. [cited 2020 May 19]; Available from: https://www.sciencedirect.com |
|
[69] |
WE FSD C, CE T. Reverse transcription-polymerase chain reaction (RT-PCR) phenotypic analysis of cell cultures of human tracheal epithelium, tracheobronchial glands, and lung carcinomas. Am J Respir Cell Mol Biol 1993; 9(5) |
|
[70] |
Wan H, Winton H, Soeller C, Stewart G, Thompson P, Gruenert D. Tight junction properties of the immortalized human bronchial epithelial cell lines Calu-3 and 16HBE14o-Tight junction properties of the immortalized human bronchial epithelial cell lines Calu-3 and 16HBE14o. Eur Respir J 2000; 15(6): 1058-68. |
|
[71] |
Shen BQ, Finkbeiner WE, Wine JJ, Mrsny RJ, Widdicombe JH. Calu-3: A human airway epithelial cell line that shows cAMP-dependent Cl- secretion. Eur Respir J 2000; 16(6): 1058-68. |
|
[72] |
Kreft ME, Jerman UD, Lasič E, et al. The characterization of the human cell line Calu-3 under different culture conditions and its use as an optimized in vitro model to investigate bronchial epithelial function. Eur J Pharm Sci 2015; 69: 1-9. https://linkinghub.elsevier.com/retri eve/pii/S0928098714004758 [Internet].[http://dx.doi.org/10.1016/j.ejps.2014.12.017] [PMID: 25555374] |
|
[73] |
Mukherjee M, Pritchard DI, Bosquillon C. Evaluation of air-interfaced Calu-3 cell layers for investigation of inhaled drug interactions with organic cation transporters in vitro . Int J Pharm 2012; 426(1-2): 7-14.https://linkinghub.elsevier.com/retrieve/pii/S0378517311011628 [Internet].[http://dx.doi.org/10.1016/j.ijpharm.2011.12.036] [PMID: 22265910] |
|
[74] |
Jeong MH, Kim HR, Bang IJ, et al. in vitro model for predicting acute inhalation toxicity by using a Calu-3 epithelium cytotoxicity assay. J Pharmacol Toxicol Methods 2019; 98: 106576.https://linkinghub.elsevier.com/retrieve/pii/S1056871918307019 [Internet].[http://dx.doi.org/10.1016/j.vascn.2019.04.002] [PMID: 31026561] |
|
[75] |
Fujii S. (BBA)-Enzymology YH-B et BA, 1981 undefined. New synthetic inhibitors of C1r, C1 esterase, thrombin, plasmin, kallikrein and trypsin. Elsevier [Internet]. [cited 2020 May 21]; Available from: https://www.sciencedirect.com/science/article/pii/0005274481900231 |
|
[76] |
Iwaki M, Ino Y, Motoyoshi A, Ozeki M, Sato T, Kurumi M. Pharmacological studies of FUT-175, nafamostat mesilate v. Effects on the Pancreatic Enzymes and Experimental Acute Pancreatitis in Rats [Internet] https://jstage.jst.go.jp. |
|
[77] |
Minakata D, Fujiwara SI, Ikeda T, et al. Comparison of gabexate mesilate and nafamostat mesilate for disseminated intravascular coagulation associated with hematological malignancies. Int J Hematol 2019; 109(2): 141-6.[http://dx.doi.org/10.1007/s12185-018-02567-w] [PMID: 30536180] |
|
[78] |
Ohtake Y, Hirasawa H, Sugai T. SO-C, 1991 undefined. Nafamostat mesylate as anticoagulant in continuous hemofiltration and continuous hemodiafiltration. karger.com [Internet]. [cited 2020 May 21]; Available from: https://www.karger.com |
|
[79] |
Yamamoto M, Kiso M, Sakai-Tagawa Y, Iwatsuki-Horimoto K, Imai M, Takeda M. The anticoagulant nafamostat potently inhibits SARS-CoV-2 infection in vitro : an existing drug with multiple possible therapeutic effects. Viruses 2020; 12(6): 629.[http://dx.doi.org/10.1101/2020.04.22.054981] |
|
[80] |
De Clercq E. Suramin: a potent inhibitor of the reverse transcriptase of RNA tumor viruses. Cancer Lett 1979; 8(1): 9-22.[http://dx.doi.org/10.1016/0304-3835(79)90017-X] [PMID: 92362] |
|
[81] |
McGeary R, Bennett A. QT-M reviews in, 2008 undefined. Suramin: clinical uses and structure-activity relationships. europepmc.org [Internet]. [cited 2020 May 22]; Available from: https://europepmc.org/abstract/med/18991754 |
|
[82] |
da Silva CSB, Thaler M, Tas A, Ogando NS, Bredenbeek PJ, Ninaber DK. Suramin inhibits SARS-CoV-2 infection in cell culture by interfering with early steps of the replication cycle bioRxiv 2020. |
|
[83] |
Ammerman NC, Beier-Sexton M, Azad AF. Growth and maintenance of vero cell lines. Curr Protoc Microbiol 2008.[http://dx.doi.org/10.1002/9780471729259.mca04es11] |
|
[84] |
Osada N, Kohara A, Yamaji T, Hirayama N, Kasai F, Sekizuka T. The Genome Landscape of the African Green Monkey Kidney-Derived Vero Cell Line [cited 2020 May 23]; Available from: http://picard.sourceforge.net[http://dx.doi.org/10.1093/dnares/dsu029] |
|
[85] |
Levenbook IS, Petricciani JC, Elisberg BL. Tumorigenicity of vero cells. J Biol Stand 1984; 12(4): 391-8.[http://dx.doi.org/10.1016/S0092-1157(84)80063-3] [PMID: 6526826] |
|
[86] |
Barrett PN, Mundt W, Kistner O, Howard MK. Vero cell platform in vaccine production: moving towards cell culture-based viral vaccines. Expert Rev Vaccines 2009; 8(5): 607-18.[http://dx.doi.org/10.1586/erv.09.19] [PMID: 19397417] |
|
[87] |
Aubrit F, Perugi F, Léon A, et al. Cell substrates for the production of viral vaccines. Vaccine 2015; 33(44): 5905-12.https://linkinghub.elsevier.com/retrieve/pii/S0264410X15009329 [Internet].[http://dx.doi.org/10.1016/j.vaccine.2015.06.110] [PMID: 26187258] |
|
[88] |
Montagnon B, Fanget B. biological AN-D in, 1981 undefined. The large-scale cultivation of VERO cells in micro-carrier culture for virus vaccine production. Preliminary results for killed poliovirus vaccine. europepmc.org [Internet]. [cited 2020 May 23]; Available from: https://europepmc.org/abstract/med/6785126 |
|
[89] |
Van Wezel A, Van Steenis G. CH-D in, 1978 undefined. New approach to the production of concentrated and purified inactivated polio and rabies tissue culture vaccines. europepmc.org [Internet]. [cited 2020 May 23]; Available from: https://europepmc.org/article/med/223908 |
|
[90] |
Vidor E, Meschievitz C. disease SP-TP infectious, 1997 undefined. Fifteen years of experience with Vero-produced enhanced potency inactivated poliovirus vaccine. [Internet] [cited 2020 May 23]; Available from: https://journals.lww.com |
|
[91] |
Rhim JS, Schell K, Creasy B, Case W. Biological characteristics and viral susceptibility of an African green monkey kidney cell line (Vero). Proc Soc Exp Biol Med 1969; 132(2): 670-8.[http://dx.doi.org/10.3181/00379727-132-34285] [PMID: 4982209] |
|
[92] |
Desmyter J, Melnick JL, Rawls WE. Defectiveness of interferon production and of rubella virus interference in a line of African green monkey kidney cells (Vero). J Virol 1968; 2(10): 955-61.[http://dx.doi.org/10.1128/jvi.2.10.955-961.1968] [PMID: 4302013] |
|
[93] |
Diaz MO, Ziemin S, Le Beau MM, et al. Homozygous deletion of the α- and β 1-interferon genes in human leukemia and derived cell lines. Proc Natl Acad Sci USA 1988; 85(14): 5259-63.[http://dx.doi.org/10.1073/pnas.85.14.5259] [PMID: 3134658] |
|
[94] |
Lokugamage KG, Hage A, Schindewolf C, Rajsbaum R, Menachery VD. SARS-CoV-2 is sensitive to type I interferon pretreatment bioRxiv 2020.[http://dx.doi.org/10.1101/2020.03.07.982264] |
|
[95] |
Mulangu S, Dodd LE, Davey RT, Jr, et al. PALM Writing GroupPALM Consortium Study TeamA randomized, controlled trial of ebola virus disease therapeutics. N Engl J Med 2019; 381(24): 2293-303.[http://dx.doi.org/10.1056/NEJMoa1910993] [PMID: 31774950] |
|
[96] |
Gordon CJ, Tchesnokov EP, Woolner E, Perry JK, Feng JY, Porter DP, et al. Remdesivir is a direct-acting anti-viral that inhibits RNA-dependent RNA polymerase from severe acute respiratory syndrome coronavirus 2 with high potency. J Biol Chem 2020 Apr 13; jbc.RA120.013679 |
|
[97] |
Choy KT, Wong AYL, Kaewpreedee P, Sia SF, Chen D, Hui KPY, et al. Remdesivir, lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro. Antiviral Res. 2020 June 1; 178: 104786 |
|
[98] |
Agostini ML, Andres EL, Sims AC, et al. Coronavirus susceptibility to the anti-viral remdesivir (GS-5734) is mediated by the viral polymerase and the proofreading exoribonuclease. MBio 2018; 9(2): e00221-18.[http://dx.doi.org/10.1128/mBio.00221-18] [PMID: 29511076] |
|
[99] |
Hurst M, Faulds D. Lopinavir. Drugs 2000; 60(6): 1371-9.[http://dx.doi.org/10.2165/00003495-200060060-00009] [PMID: 11152017] |
|
[100] |
Cvetkovic RS, Goa KL. Lopinavir/ritonavir: A review of its use in the management of HIV infection. Drugs 2003; Vol. 63: 769-802. |
|
[101] |
Mangum EM, Graham KK. Lopinavir-Ritonavir: a new protease inhibitor. Pharmacotherapy 2001; 21(11): 1352-63.http://doi.wiley.com/10.1592/phco.21.17.1352.34419 [Internet].[http://dx.doi.org/10.1592/phco.21.17.1352.34419] [PMID: 11714208] |
|
[102] |
Xiu-jin Ye, Mao-fang LinHomoharringtonine induces apoptosis of endothelium and down-regulates vegf expression of K562 cells. J Zhejiang Univ Sci 2004; 5(2): 230-4. |
|
[103] |
Dong HJ, Wang ZH, Meng W, et al. The natural compound homoharringtonine presents broad anti-viral activity in vitro and in vivo . Viruses 2018; 10(11): 601.[http://dx.doi.org/10.3390/v10110601] [PMID: 30388805] |
|
[104] |
Ianevski A, Yao R, Fenstad MH, Biza S, Zusinaite E, Lysvand H. Potential anti-viral options against SARS-CoV-2 infection bioRxiv 2020. |
|
[105] |
Akinboye ES, Bakare O. Biological activities of emetine. The Open Natural Products Journal 2011; 4: 8-15.[http://dx.doi.org/10.2174/1874848101104010008] |
|
[106] |
Yang S, Xu M, Lee EM, et al. Emetine inhibits Zika and Ebola virus infections through two molecular mechanisms: inhibiting viral replication and decreasing viral entry. Cell Discov 2018; 4(1): 31.[http://dx.doi.org/10.1038/s41421-018-0034-1] [PMID: 29872540] |
|
[107] |
Campbell WC. Ivermectin: an update. Parasitol Today 1985; 1(1): 10-6.[http://dx.doi.org/10.1016/0169-4758(85)90100-0] [PMID: 15275618] |
|
[108] |
Campbell WC, Fisher MH, Stapley EO, Albers-Schönberg G, Jacob TA. Ivermectin: A potent new antiparasitic agent. Science (80- ) [Internet] 1983; 221(4613): 8-823.[http://dx.doi.org/10.1126/science.6308762] |
|
[109] |
Caly L, Druce JD, Catton MG, Jans DA, Wagstaff KM. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro . Antiviral Res 2020; 178: 104787.[http://dx.doi.org/10.1016/j.antiviral.2020.104787] [PMID: 32251768] |
|
[110] |
Yang SNY, Atkinson SC, Wang C, et al. The broad spectrum antiviral ivermectin targets the host nuclear transport importin α/β1 heterodimer. Antiviral Res 2020; 177: 104760. https://linkinghub.elsevier.com/retri eve/pii/S0166354219307211 [Internet].[http://dx.doi.org/10.1016/j.antiviral.2020.104760] [PMID: 32135219] |
|
[111] |
Liu J, Cao R, Xu M, Wang X, Zhang H, Hu H. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. naturecom [Internet] [cited 2020 May 29]; Available from: https://www.nature.com |
|
[112] |
Al-Bari MAA. Targeting endosomal acidification by chloroquine analogs as a promising strategy for the treatment of emerging viral diseases. Pharmacol Res Perspect 2017; 5(1): e00293.[http://dx.doi.org/10.1002/prp2.293] [PMID: 28596841] |
|
[113] |
Zhou D, Dai S. Antimicrobial QT-J of, 2020 undefined. COVID-19: a recommendation to examine the effect of hydroxychloroquine in preventing infection and progression. academic.oup.com [Internet]. [cited 2020 May 29]; Available from: https://academic.oup.com |
|
[114] |
Wang M, Cao R, Zhang L, Yang X, Liu J, Xu M. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus. Cell Res 2020; 30(3): 269-71. |
|
[115] |
Liu J, Cao R, Xu M, Wang X, Zhang H, Hu H. Hydroxychloroquine, a less toxic derivative of chloroquine, is effective in inhibiting SARS-CoV-2 infection in vitro. Cell Discovery Springer Nature 2020; 6: 1-4. |
|
[116] |
Bardsley-Elliot A, Plosker CL. Nelfinavir: An update on its use in HIV infection 2000; 59: 581-620. |
|
[117] |
Jarvis B, Faulds D. A review of its therapeutic efficacy in HIV infection. Drugs 1998; Vol. 56: 67-147. |
|
[118] |
Koltai T. Nelfinavir and other protease inhibitors in cancer: Mechanisms involved in anticancer activity. F1000Research 2015; Vol. 4 |
|
[119] |
Xu Z, Yao H, Shen J, Wu N, Xu Y, Lu X. Nelfinavir Is Active Against SARS-CoV-2 in Vero E6 Cells. ChemRxiv 2020.https://chemrxiv.org/articles/Nelfinavir_Is_Active_Against_SARS-CoV-2_in_Vero_E6_Cells/12039888/1 |
|
[120] |
Musarrat F, Chouljenko V, Dahal A, Nabi R, Chouljenko T, Jois SD. The anti HIV drug nelfinavir mesylate (Viracept) is a potent inhibitor of cell fusion caused by the SARSCoV 2 spike (S) glycoprotein warranting further evaluation as an anti viral against COVID-19 infections. J Med Virol [Internet] 2020 May 17 [cited 2020 May 30]; jmv.25985. Available from: https://onlinelibrary.wiley.com |
|
[121] |
Yamamoto N, Matsuyama S, Hoshino T, Yamamoto N. Nelfinavir inhibits replication of severe acute respiratory syndrome coronavirus 2 in vitro. bioRxiv 2020. |
|
[122] |
Summ O, Andreou AP, Akerman S, Goadsby PJ. A potential nitrergic mechanism of action for indomethacin, but not of other COX inhibitors: relevance to indomethacin-sensitive headaches. J Headache Pain 2010; 11(6): 477-83. https://thejournalofheadacheandpain.biomedcentral.com /articles/10.1007/s10194-010-0263-7 [Internet].[http://dx.doi.org/10.1007/s10194-010-0263-7] [PMID: 20978816] |
|
[123] |
Summ O, Evers S. Mechanism of action of indomethacin in indomethacin-responsive headaches. Curr Pain Headache Rep 2013; 17(4): 327.[http://dx.doi.org/10.1007/s11916-013-0327-x] [PMID: 23423598] |
|
[124] |
Martella V, Decaro N. Indomethacin has a potent anti-viral activity against SARS coronavirus [Internet]. 2006 [cited 2020 May 30]. Available from: https://www.researchgate.net /publication/6503810 |
|
[125] |
Xu T, Gao X, Wu Z, Selinger DW, Zhou Z. Indomethacin has a potent anti-viral activity against SARS CoV-2 in vitro and canine coronavirus in vivo. bioRxiv 2019. https://www.biorxiv.org/content/10.1101 /2020.04.01.017624v1 |
|
[126] |
Gomeni R, Xu T, Gao X. Françoise Bressolle-Gomeni. Model based approach for estimating the dosage regimen of indomethacin a potential anti-viral treatment of patients infected with SARS CoV-2. J Pharmacokinet Pharmacodyn 2020; 43(3): 189-98.[http://dx.doi.org/10.1007/s10928-020-09690-4] [PMID: 32435882] |
|
[127] |
Rustgi VK, Lee WM, Lawitz E, et al. MErimepodib TRiple cOmbination Study GroupMerimepodib, pegylated interferon, and ribavirin in genotype 1 chronic hepatitis C pegylated interferon and ribavirin nonresponders. Hepatology 2009; 50(6): 1719-26.[http://dx.doi.org/10.1002/hep.23204] [PMID: 19852040] |
|
[128] |
Li S fang, Gong M jiao, Shao J jun, Sun Y feng, Zhang Y guang, Chang H yun. Anti-viral activity of merimepodib against foot and mouth disease virus in vitro and in vivo. Mol Immunol 2019; 114: 226-32.https://linkinghub.elsevier.com/retrieve/pii/S0161589019301774 [Internet].[http://dx.doi.org/10.1016/j.molimm.2019.07.021] |
|
[129] |
Tong X, Smith J, Bukreyeva N, et al. Merimepodib, an IMPDH inhibitor, suppresses replication of Zika virus and other emerging viral pathogens. Antiviral Res 2018; 149: 34-40.https://linkinghub.elsevier.com/retrieve/pii/S0166354217302371 [Internet].[http://dx.doi.org/10.1016/j.antiviral.2017.11.004] [PMID: 29126899] |
|
[130] |
Bukreyeva N, Mantlo EK, Sattler RA, Huang C, Paessler S, Zeldis J. The IMPDH inhibitor merimepodib suppresses SARS-CoV-2 replication in vitro bioRxiv. |
|
[131] |
Gao Z, Huang K, Xu H. Protective effects of flavonoids in the roots of Scutellaria baicalensis Georgi against hydrogen peroxide-induced oxidative stress in HS-SY5Y cells. Pharmacol Res 2001; 43(2): 173-8.[http://dx.doi.org/10.1006/phrs.2000.0761] [PMID: 11243719] |
|
[132] |
H Bin Li, Y Jiang, F Chen. Separation methods used for Scutellaria baicalensis active components. Journal of Chromatography B: Analytical Technologies in the Biomedical and Life Sciences 2004; 812: 90-277.[http://dx.doi.org/] [PMID: ] |
|
[133] |
Liu H, Ye F, Sun Q, Liang H, Li C, Lu R, et al. Scutellaria baicalensis extract and baicalein inhibit replication of SARS-CoV-2 and its 3C-like protease in vitro J Enzyme Inhib Med Chem 2021; 36(1): 497-503. [http://dx.doi.org/10.1101/2020.04.10.035824] |
|
[134] |
S Noble, KL Goa. Gemcitabine A review of its pharmacology and clinical potential in non-small cell lung cancer and pancreatic cancer 199772-447. |
|
[135] |
Lawrence TS, Eisbruch A, Mcginn CJ, Fields MT, Shewach DS. Radiosensitization by gemcitabine published on physicians practice. 1999 [cited 2020 Jun 1]. Available from: http://www.physicianspractice.com |
|
[136] |
Lee K, Kim D eun, Jang KS, Kim SJ, Cho S, Kim C. Gemcitabine, a broad-spectrum anti-viral drug, suppresses enterovirus infections through innate immunity induced by the inhibition of pyrimidine biosynthesis and nucleotide depletion. Oncotarget 2017; 8(70): 115315-25.[http://dx.doi.org/10.18632/oncotarget.23258] [PMID: 29383162] |
|
[137] |
Gemcitabine, lycorine and oxysophoridine inhibit novel coronavirus (SARS-CoV-2) in cell culture. Emerg Microbes Infect [Internet] 2020 May 20 [cited 2020 June 1];1–10. Available from: https://www.tandfonline.com/doi/full/10.1080/22221751.2020.1772676 |
|
[138] |
Zhang P, Liu S. Solvent Effects on the UV Absorption Spectrum of Carmofur. Detection [Internet]. 2016 [cited 2020 June 1];4:25–31. Available from: http://www.scirp.org |
|
[139] |
Domraceva I, Petrova M, Duburs G. 2-Dimyristoyl-sn-glycero-3-phosphocholine (DMPC) increases Carmofur stability and in vitro antiproliferative effect Cardiovascular drugs View project Inhibitors of multidrug resistance View project. [cited 2020 June 1] :http://dx.doi.org/doi:10.1016/j.toxrep.2015.01.009 |
|
[140] |
Govindarajah N, Clifford R, Bowden D, Sutton PA, Parsons JL, Vimalachandran D. Sphingolipids and acid ceramidase as therapeutic targets in cancer therapy Internet2019; Vol. 138: 104-11. https://linkinghub.elsevier.com/retri eve/pii/S1040842818305079 |
|
[141] |
Khaerunnisa S, Kurniawan H, Awaluddin R, Suhartati S. Potential Inhibitor of COVID-19 Main Protease (M pro) from Several Medicinal Plant Compounds by Molecular Docking Study Preprints 2020. https://www.preprints.org/manuscript/202003.0226/v1 |
|
[142] |
Jin Z, Zhao Y, Sun Y, et al. Structural basis for the inhibition of SARS-CoV-2 main protease by antineoplastic drug carmofur. Nat Struct Mol Biol 2020; 27(6): 529-32.[http://dx.doi.org/10.1038/s41594-020-0440-6] [PMID: 32382072] |
|
[143] |
Leneva IA, Russell RJ, Boriskin YS, Hay AJ. Characteristics of arbidol-resistant mutants of influenza virus: implications for the mechanism of anti-influenza action of arbidol. Antiviral Res 2009; 81(2): 132-40. https://linkinghub.elsevier.com/retri eve/pii/S0166354208004312 [Internet].[http://dx.doi.org/10.1016/j.antiviral.2008.10.009] [PMID: 19028526] |
|
[144] |
Blaising J, Polyak SJ, Pécheur EI. Arbidol as a broad-spectrum anti-viral: An update. Antiviral Research 2014; Vol. 107: 84-94. |
|
[145] |
Boriskin YS, Leneva IA, Pécheur E-I, Polyak SJ. Arbidol: a broad-spectrum antiviral compound that blocks viral fusion. Curr Med Chem 2008; 15(10): 997-1005.[http://dx.doi.org/10.2174/092986708784049658] [PMID: 18393857] |
|
[146] |
Wang X, Cao R, Zhang H, Liu J, Xu M, Hu H. The anti-influenza virus drug, arbidol is an efficient inhibitor of SARS-CoV-2 in vitro 2020; Vol. 6: 1-5. |